Ketogenic Diet Helps Treat Rare Condition Known as "Glut 1"
Reed Williams was seemingly healthy the first 12 months of life, but shortly after his first birthday, he was sitting at the dinner table one night when suddenly his whole body drooped to one side.
“We knew something was terribly wrong,” said his mother, Anna Williams. His father, Jason Williams, a firefighter/paramedic agreed. Based on his experience, it seemed like Reed was having a stroke.
“All I could think was, ‘There’s no way. He’s just one year old,’” Jason said.
The Williams family called 911 for help. At Children’s Mercy, testing confirmed the episode was a seizure, not a stroke.
“During these seizures, Reed would look like he was sleeping with his eyes wide open. He had no response to you whatsoever,” Jason said. But why was Reed was having these seizures, sometimes hundreds of times a day?
“The only test that was abnormal the first night in the emergency room was Reed’s cerebral spinal fluid,” Jason said. “The glucose in his spinal fluid was significantly lower than it should have been.”
Initially, doctors prescribed anti-seizure medications for Reed, but they didn’t help. In fact, the toddler’s development seemed to be regressing.
Suspecting Glut1
Reed’s pediatric neurologist at Children’s Mercy suspected he might have a rare condition called Glucose Transporter Type 1 Deficiency Syndrome, or Glut1. A second spinal tap several weeks later confirmed the doctor’s suspicions.
“Being diagnosed with Glut1 is like finding a needle in a haystack,” Jason said. “It’s such a rare condition.”
At the time, Reed was only 18 months old, and one of just a couple hundred people in the world with the genetic disorder which impairs brain metabolism. With Glut1, glucose isn’t transported properly into the brain, leaving it starving for the energy necessary to grow and function.
According to the Glut1 Deficiency Foundation, more than 100 different types of mutations and deletions of this gene have been found to date. Approximately 90 percent of affected individuals have frequent seizures beginning in the first months of life.
Reed’s pediatric neurologist recommended the family try the ketogenic diet to treat the toddler, and they agreed. The ketogenic diet is the recommended standard treatment for Glut1. The diet helps improve symptoms for most patients by giving the brain an alternate source of energy, and helps optimize brain growth and development.
The Children’s Mercy Ketogenic Diet Program
Reed was admitted to the hospital for three days to put him into ketosis, a metabolic state in which some of the body's energy supply comes from ketone bodies in the blood. The ketogenic diet is high in fat, moderate in protein, and low in carbohydrates. It’s a major lifestyle change that requires the full commitment of patients and their families.
“He wasn’t walking and could only say about 25 words when we started the diet,” Anna said. “Overnight, we could tell there was a difference in his gross and fine motor skills. He became more alert, his coloring improved and so did his vocabulary. He became a kid again!”
“Reed was one of the very first to be on the diet for Glut1 at Children’s Mercy,” Jason said. “The results were like night and day!”
That was eight years ago, and the ketogenic diet program at Children’s Mercy also was in its infancy.
“Reed’s dietitian, Lindsey Thompson, helped us with recipes and made sure Reed was getting a nutritionally balanced diet, but it was a challenge at times,” Anna said. “At that point, there weren’t any cooking classes, and the diet options were limited.”
Today the Children’s Mercy team includes a physician or nurse practitioner, staff nurses, social workers, dietitians and a chef educator who teaches keto cooking classes for patients and families. After admission, the family has regular contact with the support team to ensure all dietary needs are being met, including meal changes. The family also has access to group and individual support services.
Stick to It!
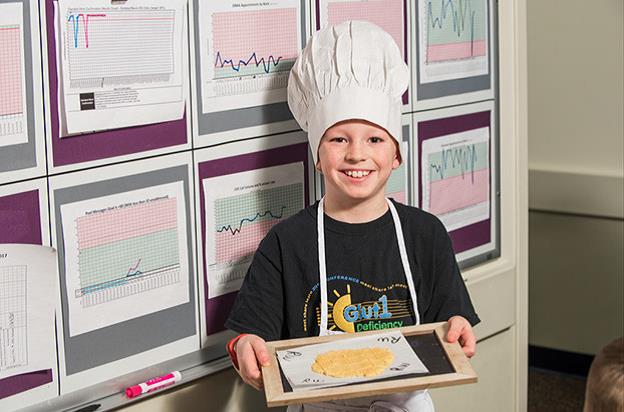
Chef Rachel Finn Emily Williams, Reed Williams, Chef Rachel
Though sticking to the diet has been tough, the Williams family has done it. And with help from speech, occupational and physical therapies, Reed has caught back up developmentally with his peers.
Now a third grader at Piper Elementary School, Reed continues to thrive, in spite of being diagnosed with Glut1. Like most 9 1/2-year-old boys, he likes playing outside, but he also enjoys cooking classes with Chef Rachel Finn.
“I like the food we make,” Reed said. “Tomato soup is one of my favorites.”
Reed’s stepmom, Emily Williams, also enjoys cooking and helping Reed with the diet, altering recipes to make his favorites keto-friendly.
“Emily made a great chocolate chip cookie recipe that she shared with the cooking class,” Anna said. “That was a big hit.” Plus, there are lots of other resources now available, like Pinterest and websites, that make preparing keto-friendly meals easier.
Anna’s advice to parents whose children are prescribed the ketogenic diet is to give it a chance.
“It can be overwhelming, but it’s worth it,” Anna said. “It’s a complete lifestyle change, but use your resources. The hospital team is there for you. The diet can become your new normal.”
“We have a phenomenal hospital and ketogenic diet program here,” Jason added. “There are people who travel hours to get to a hospital that delivers the quality of care we have at Children’s Mercy. We are very fortunate. The nursing staff, doctors, nutritionists, and Chef Rachel, are amazing.”
Learn more about the Ketogenic Diet Program at Children's Mercy.